Your Ingrown Toenail Is Not “Just a Bad Nail” When DIY Goes Wrong
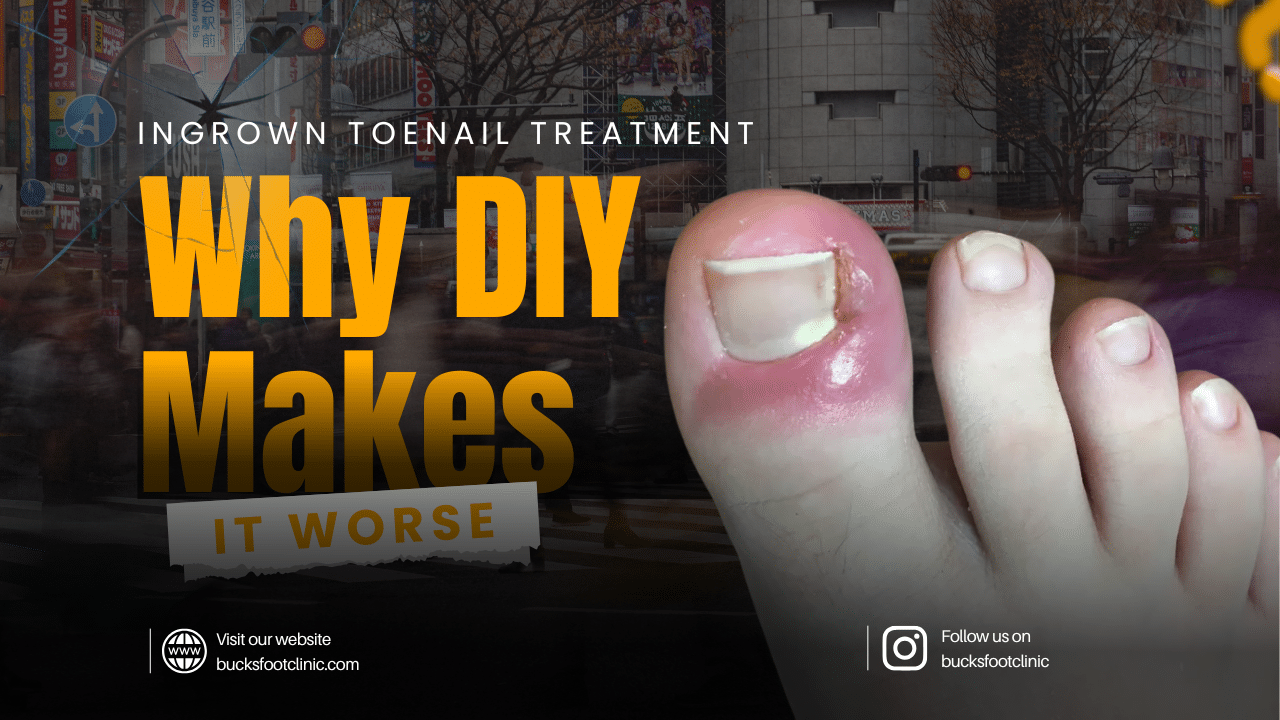
It starts with a niggle. A bit of tenderness along the side of your big toe. You think it’ll sort itself out, so you leave it. A few days later, it’s red, swollen, and throbbing. You grab the nail clippers and try to dig out the offending edge yourself in the bathroom, and that’s where the real trouble begins. Ingrown toenail treatment is one of the most common reasons people visit Bucks Foot Clinic, and in the majority of cases, patients come to us after DIY attempts have turned a minor problem into a painful, infected mess.
This isn’t a criticism. It’s completely natural to try to sort it yourself first. But understanding why home treatment so often makes things worse can save you weeks of unnecessary pain.
What Causes Ingrown Toenails?
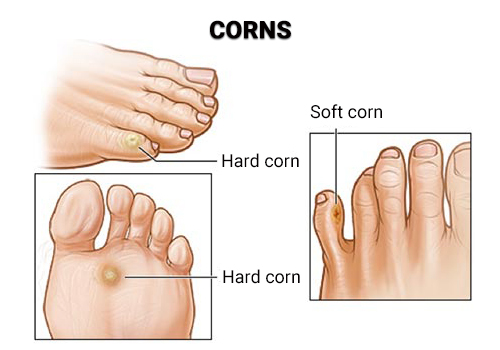
An ingrown toenail occurs when the edge or corner of a toenail grows into the surrounding skin, causing pain, swelling, and sometimes infection. The big toe is most commonly affected, though any toenail can become ingrown.
Several factors contribute to ingrown toenails developing. Cutting nails too short or rounding the corners encourages the nail to grow into the skin as it regrows. Tight or narrow footwear presses the toes together, forcing the nail edge into the flesh. Trauma to the toe, such as stubbing it, dropping something on it, or repetitive pressure from sports, can alter nail growth. Some people are simply genetically predisposed to curved nails that are more likely to become ingrown. Sweaty feet soften the skin around the nail, making it easier for the nail edge to penetrate. Pedicures performed incorrectly (cutting too short, rounding corners, aggressive cuticle work) are another common cause.
Why DIY Treatment Usually Makes It Worse
When you try to cut out an ingrown toenail at home, several things typically go wrong. First, you can’t see what you’re doing clearly enough the affected area is swollen, tender, and difficult to access. Second, bathroom nail clippers aren’t designed for precision work on an embedded nail edge. Third, and most importantly, you almost always leave behind a small spike or spicule of nail that you can’t see or feel at the time.
This tiny remnant continues growing into the skin, now in a deeper, more problematic position than before. The wound you’ve created from your DIY attempt also provides an open door for bacteria, leading to infection. What started as mild discomfort becomes a red, swollen, pus-filled toe that’s significantly more painful and more complicated to treat than the original ingrown nail.
Cotton wool wedged under the nail, repeated soaking, and antiseptic cream can help manage symptoms temporarily, but none of these address the underlying problem: a nail edge that’s growing where it shouldn’t be.
Struggling with this problem? Call Bucks Foot Clinic on 01494 434366 or book online at bucksfootclinic.com for expert advice and treatment.
How to Prevent Ingrown Toenails
- Cut your toenails straight across, never curved or rounded at the corners this is the single most effective prevention measure
- Don’t cut nails too short; leave them level with the tip of the toe (approximately 1–2mm of white nail visible)
- Use proper nail clippers or nippers designed for toenails, not small fingernail scissors
- Wear shoes with adequate room in the toe box your toes should never feel squeezed or compressed
- Keep feet clean and dry to prevent the surrounding skin from softening excessively
- If you have pedicures, ensure the technician cuts nails straight across and doesn’t round the corners
- Protect your toes during sport with appropriate footwear runners and footballers are particularly prone
- If you notice early signs of an ingrown nail (tenderness, slight redness), don’t ignore it early professional intervention is simpler and less painful than treating an established infection
Why a Podiatrist Gets Better Results Than Home Ingrown Toenail Treatment
A podiatrist has the training, tools, and clinical environment to resolve ingrown toenails safely and effectively. Here’s what makes professional treatment fundamentally different from DIY:
- We can see the full extent of the problem using proper lighting and magnification, identifying embedded nail spicules that are invisible to the naked eye
- Sterile instruments designed specifically for nail work allow precise removal of the offending nail edge without damaging surrounding tissue
- If infection is present, we can assess its severity and provide appropriate treatment, including antibiotics if necessary
- For recurrent ingrown toenails, we offer a minor procedure called partial nail avulsion that provides a permanent solution
- Professional treatment is performed under local anaesthetic meaning the procedure itself is painless, unlike the excruciating experience of digging at an inflamed toe with nail clippers
Don’t suffer with a painful ingrown toenail any longer. Contact Bucks Foot Clinic today on 01494 434366 to book your appointment, or visit bucksfootclinic.com. We have clinics in Amersham, Chesham, and Little Chalfont.
How Bucks Foot Clinic Fixes Ingrown Toenail Treatment
Conservative treatment
For mild ingrown toenails caught early, we can often resolve the problem in a single appointment by carefully removing the offending nail edge using specialist instruments under sterile conditions. This is quick, precise, and provides immediate relief.
Partial nail avulsion (for recurrent cases)
If your ingrown toenail keeps coming back, partial nail avulsion is the gold standard treatment. Performed under local anaesthetic so you won’t feel a thing, the procedure involves removing the problematic section of nail and applying a chemical (phenol) to the nail matrix to prevent that section from regrowing. The nail heals slightly narrower but looks perfectly normal. Success rates exceed 95%, and recurrence is rare.
The entire procedure takes around 30 minutes, and most patients are back in normal footwear within a few days. We provide comprehensive aftercare instructions and follow-up appointments to ensure healing progresses smoothly.
What to expect at your appointment
We understand that the thought of someone working on an already painful toe can be anxiety-inducing. Rest assured we anaesthetise the toe first, so the procedure itself is completely painless. Our podiatrists talk you through every step, and we’ve treated thousands of ingrown toenails. You’re in experienced, gentle hands.


































































































Recent Comments