Why Does My Heel Hurt First Thing in the Morning? The Truth About Plantar Fasciitis
Your alarm goes off. You swing your legs out of bed, plant your feet on the floor, and the moment you stand up, a sharp, stabbing pain shoots through your heel. You hobble to the bathroom like you’ve aged thirty years overnight. Sound familiar? If this plantar fasciitis morning heel pain has become your daily routine, you’re far from alone. Plantar fasciitis is the single most common cause of heel pain in the UK, and it affects roughly one in ten people at some point during their lifetime.
The good news? It’s entirely treatable. The bad news? Most of the advice you’ll find online either doesn’t work or actively makes things worse. Let’s separate the facts from the myths and get you back on your feet, literally.
What Actually Is Plantar Fasciitis?
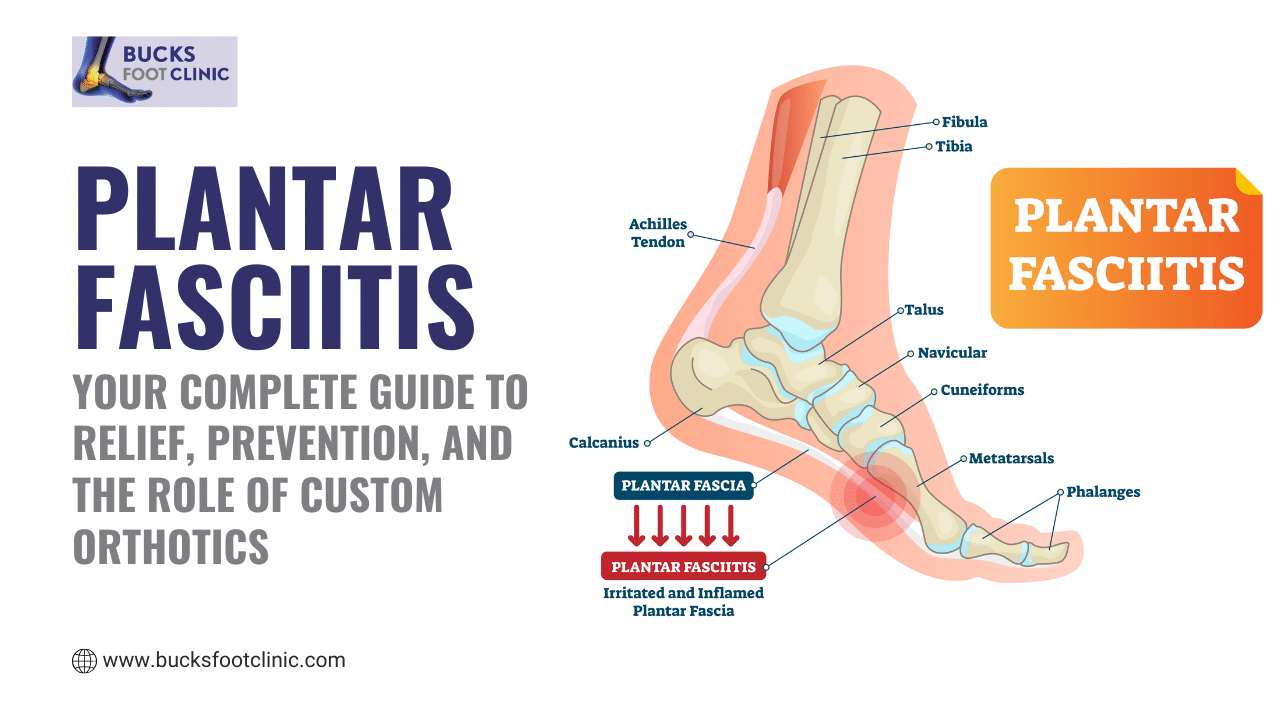
The plantar fascia is a thick, fibrous band of tissue that runs along the sole of your foot, connecting your heel bone to your toes. Think of it like a bowstring supporting the arch of your foot. Every time you take a step, this tissue absorbs shock, supports your weight, and helps propel you forward.
When the plantar fascia becomes irritated or develops tiny tears, usually from repetitive strain or excessive pressure, it thickens, tightens, and becomes painful. This is plantar fasciitis. The term technically means inflammation, although modern research suggests it’s more accurately a degenerative condition, with the tissue breaking down rather than simply swelling up.
Why Does It Hurt More in the Morning?
This is the question everyone asks, and the answer is wonderfully logical once you understand it. While you sleep, your foot relaxes into a pointed-toe position. In this position, the plantar fascia shortens and tightens overnight, almost like a rubber band that’s been held slack for hours. The moment you stand up and flatten your foot against the floor, that tightened fascia is suddenly stretched under your full body weight. The result is that characteristic stabbing pain with your first steps.
The same mechanism explains why pain returns after sitting for long periods. Any time the fascia shortens during rest and then gets rapidly loaded, it protests. As you walk around and the tissue gradually warms up and stretches, the pain typically eases only to return after your next period of rest.
Common Myths About Plantar Fasciitis
Myth 1: Heel spurs cause the pain
Many people receive an X-ray showing a heel spur and assume that’s the source of their agony. In reality, heel spurs are found in many people who have absolutely no pain at all. The spur forms as a response to stress on the heel, but it’s rarely the actual cause of your discomfort. Treating the spur alone won’t fix the problem.
Myth 2: You just need to rest
Complete rest might sound logical, but plantar fasciitis is one of those frustrating conditions where doing nothing can actually make things worse. The tissue needs controlled, gradual loading to heal properly. Total rest allows the fascia to tighten further, meaning your first steps after resting are even more painful.
Myth 3: Any insole will help
Grabbing a £10 gel insole from the pharmacy might provide temporary cushioning, but it cannot correct the biomechanical issues that caused your plantar fasciitis in the first place. Generic insoles are designed for average feet. Your feet aren’t average they’re uniquely yours, with their own arch height, gait pattern, and pressure points.
Struggling with this problem? Call Bucks Foot Clinic on 01494 434366 or book online at bucksfootclinic.com for expert advice and treatment.
How to Prevent Plantar Fasciitis
- Wear supportive footwear with good arch support and cushioned soles avoid walking barefoot on hard floors, especially first thing in the morning
- Replace worn-out trainers regularly, particularly if you run or walk frequently (every 400–500 miles is the general guideline)
- Maintain a healthy weight to reduce the load on your plantar fascia with every step
- Stretch your calves and feet daily, especially before and after exercise tight calf muscles are one of the biggest contributing factors
- Increase activity levels gradually rather than making sudden jumps in distance or intensity
- Avoid prolonged standing on hard surfaces without breaks if your job requires it, invest in proper supportive footwear or an anti-fatigue mat
- Strengthen the intrinsic muscles of your feet with towel scrunches and marble pickups
Why Home Remedies Fall Short
If you’ve been rolling a frozen water bottle under your foot, stretching your calves against a wall, and hoping for the best, you’re doing the right things but likely not enough. Home remedies address symptoms without identifying the root cause. Plantar fasciitis develops for a reason: it might be flat feet causing excessive pronation, tight calf muscles altering your gait, or a sudden increase in activity your body wasn’t prepared for.
Without understanding why your plantar fascia became overloaded, you’re treating the effect whilst ignoring the cause. This is why so many people experience the condition repeatedly. A podiatrist doesn’t just treat your heel pain they investigate the biomechanical chain that led to it.
Why See a Podiatrist for Plantar Fasciitis
- Accurate diagnosis — your heel pain might not actually be plantar fasciitis. Conditions like Achilles tendinopathy, stress fractures, tarsal tunnel syndrome, and fat pad atrophy all mimic similar symptoms. A podiatrist can differentiate between these and ensure you receive the correct treatment.
- Biomechanical assessment — a thorough gait analysis reveals hidden issues like overpronation, leg length discrepancy, or muscle imbalances that generic advice simply cannot identify.
- Bespoke orthotics — custom-made insoles designed specifically for your feet redistribute pressure, support your arch correctly, and address the underlying mechanical fault driving your condition.
- Advanced treatments — professional options such as shockwave therapy, ultrasound-guided treatments, and structured rehabilitation programmes have significantly higher success rates than home care alone.
- Faster recovery — with professional guidance, most patients see meaningful improvement within weeks rather than the months (or years) that self-management often takes.
How Bucks Foot Clinic Treats Plantar Fasciitis
At Bucks Foot Clinic, we begin with a comprehensive assessment of your foot mechanics, medical history, and lifestyle. We examine how you walk, assess your foot posture, and identify the specific factors driving your heel pain. From there, we create a tailored treatment plan that may include:
- Bespoke orthotics crafted to your exact foot shape and biomechanical needs
- Targeted stretching and strengthening programmes designed for your specific muscle imbalances
- Shockwave therapy for chronic cases that haven’t responded to conservative treatment
- Footwear advice tailored to your lifestyle, whether you’re a runner, a nurse on twelve-hour shifts, or someone who spends most of their day at a desk
- Ongoing support and follow-up to ensure your recovery stays on track
Plantar fasciitis doesn’t have to define your mornings. With the right diagnosis and professional treatment, the vast majority of patients recover fully and return to all the activities they love.
Don’t let heel pain control your life. Contact Bucks Foot Clinic today on 01494 434366 to book your appointment, or visit bucksfootclinic.com. We have clinics in Amersham, Chesham, and Little Chalfont.













































































Recent Comments