
Heel pain is one of those problems that people often ignore at first. It may begin as a mild ache when you step out of bed in the morning or a sharp discomfort after standing up from a chair. Over time, that small pain can turn into something that affects your walk, your posture, your ability to exercise, and even your mood. For many people, heel pain slowly becomes a daily struggle.
Heel pain is incredibly common and affects people of all ages. In fact, nearly one in ten people will experience heel pain at some point in their lives. Despite how common it is, heel pain is frequently misunderstood. Many people believe heel spurs are always the cause, while others assume rest alone will fix the problem. Unfortunately, these assumptions often delay proper treatment and allow the condition to worsen.
At Bucks Foot Clinic, we regularly see patients who have lived with heel pain for months sometimes even years before seeking professional help. The good news is that with accurate diagnosis and the right treatment plan, most heel pain can be effectively resolved.
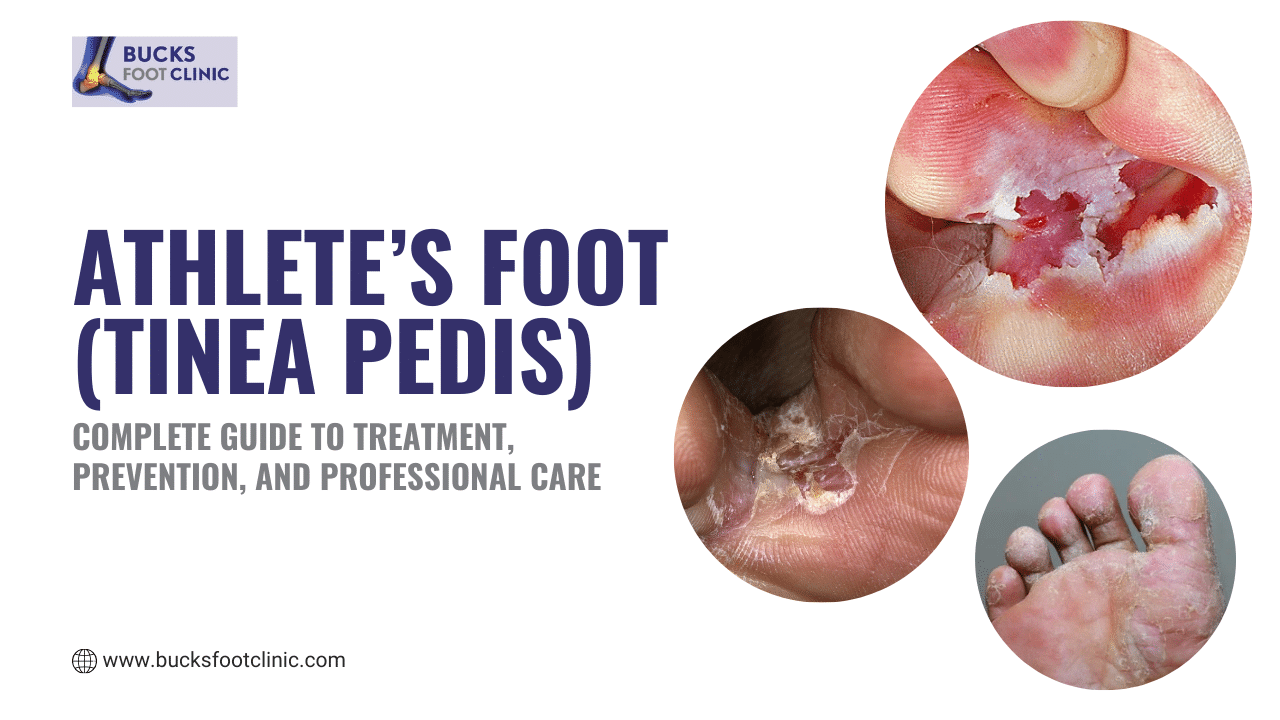
If you’re struggling with persistent itching, burning, or peeling skin on your feet, don’t let this uncomfortable condition control your life. Contact Bucks Foot Clinic on 01494 434366 today for expert assessment and effective treatment. Our experienced podiatrists specialise in eliminating athlete’s foot and preventing its return.
Understanding Heel Pain: Why It’s Not Just One Condition
Heel pain is not a diagnosis in itself. It is a symptom that can arise from several different structures within the foot. The heel is a complex area made up of bone, ligaments, tendons, cushioning tissue, nerves, and blood vessels. Any of these structures can become irritated or overloaded, leading to pain.
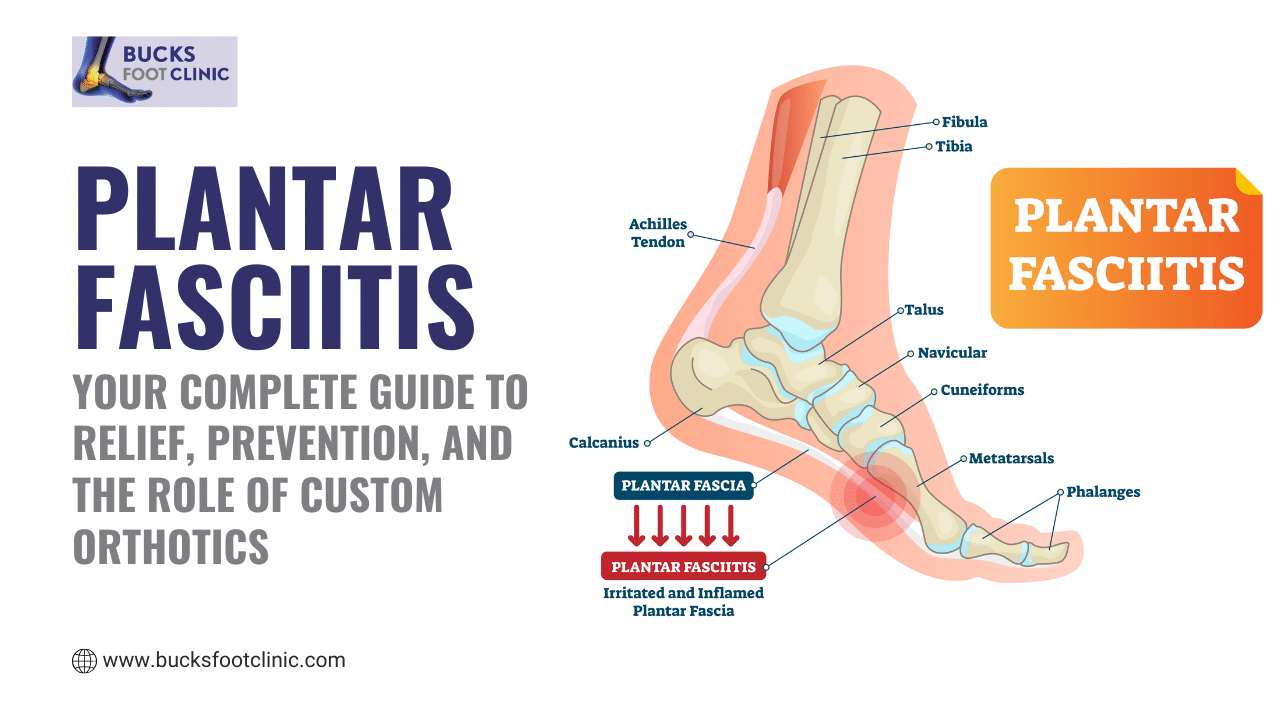
The heel bone, known as the calcaneus, absorbs a huge amount of force every time you walk. The plantar fascia, a strong band of tissue running from the heel to the toes, helps support the arch and stabilise the foot. The Achilles tendon connects the calf muscles to the heel bone and plays a vital role in walking, running, and standing. Beneath the heel lies a specialised fat pad designed to cushion impact. When any of these components stop working optimally, pain develops.
Because so many different tissues are involved, two people with heel pain may have completely different underlying problems. This is why treatments that help one person may do nothing for another.
Want personalised advice on preventing athlete’s foot based on your specific lifestyle and risk factors? Call Bucks Foot Clinic on 01494 434366 to schedule a foot health consultation. We’ll assess your individual risks and create a tailored prevention strategy.
The Most Common Causes of Heel Pain
The leading cause of heel pain is plantar fasciitis, which accounts for the majority of cases seen in podiatry clinics. This condition occurs when the plantar fascia becomes overloaded due to repeated strain. Pain is typically felt under the heel and is often worst during the first steps in the morning or after long periods of rest.
Another frequently mentioned cause is heel spurs. Heel spurs are bony growths that form gradually on the underside of the heel bone. While they are commonly blamed for pain, research shows that heel spurs themselves are rarely the true cause. Many people have heel spurs visible on X-rays and experience no pain at all.
Other causes of heel pain include thinning or damage to the heel’s fat pad, Achilles tendon problems, inflammation of bursae at the back of the heel, stress fractures, nerve compression, and inflammatory conditions such as arthritis. In children and adolescents, heel pain is often related to growth plate irritation known as Sever’s disease.
Identifying the exact cause is essential, as each condition requires a different treatment approach.
Struggling with persistent or recurrent athlete’s foot that won’t respond to over-the-counter treatments? Stop the cycle of recurrence. Call Bucks Foot Clinic on 01494 434366 today for comprehensive assessment and effective treatment. We’ll identify why it keeps coming back and create a plan to eliminate it for good.
The Truth About Heel Spurs
Heel spurs are one of the most misunderstood foot conditions. Many people imagine the spur acting like a sharp object that digs into the foot with every step. In reality, heel spurs develop slowly over time as the foot adapts to ongoing stress. They usually point forward rather than downward and do not “stab” into surrounding tissue.
Studies show that up to 20 percent of people without any heel pain have heel spurs visible on imaging. At the same time, many people suffering from severe heel pain show no evidence of a spur at all. The presence or size of a heel spur does not correlate with pain severity.
When heel pain and heel spurs exist together, the pain almost always originates from soft tissue strain, most commonly plantar fasciitis. This is why removing a heel spur surgically rarely provides relief. Treating the underlying biomechanical problem is far more effective than focusing on the spur itself.
Ready to eliminate athlete’s foot once and for all? Call Bucks Foot Clinic on 01494 434366 to schedule your comprehensive assessment. Our podiatrists will diagnose your specific type of athlete’s foot, create an effective treatment plan, and help you prevent recurrence with evidence-based strategies.
How Heel Pain Feels and Why Symptoms Matter
Heel pain does not feel the same for everyone. Some people experience a sharp, stabbing pain under the heel, while others describe a deep ache or a bruised sensation. Pain at the back of the heel may worsen with walking uphill or climbing stairs, while burning or tingling sensations may suggest nerve involvement.
The timing of pain also provides valuable clues. Pain that is worst with the first steps after rest is a classic sign of plantar fasciitis. Pain that worsens with activity and improves with rest may indicate a stress fracture or tendon problem. Constant pain, especially at night, should always be assessed promptly as it may indicate a more serious condition.
Ignoring these patterns can delay diagnosis and prolong recovery.
Don’t let athlete’s foot control your life. Take the first step towards healthy, comfortable feet today. Call Bucks Foot Clinic on 01494 434366 to schedule your comprehensive athlete’s foot assessment. Our experienced podiatrists will accurately diagnose your condition, create an effective treatment plan, and help you maintain healthy feet for the long term.
Why Heel Pain Often Becomes Chronic
One of the most frustrating aspects of heel pain is how often it becomes long-term. Many people rely on home remedies such as rest, ice, painkillers, or generic insoles. While these measures may reduce symptoms temporarily, they rarely address the underlying cause.
Most heel pain is linked to biomechanical issues, such as flat feet, high arches, poor gait mechanics, or tight calf muscles. When these issues are not corrected, the heel continues to absorb excessive stress during everyday activities. As a result, pain returns as soon as normal movement resumes.
This cycle is why heel pain frequently becomes chronic and increasingly difficult to treat without professional intervention.
The Importance of Professional Diagnosis
Seeing a podiatrist is one of the most important steps in resolving heel pain. Accurate diagnosis ensures that treatment targets the true cause rather than just masking symptoms.
At Bucks Foot Clinic, our assessment includes a detailed clinical examination, gait analysis, and biomechanical evaluation. When necessary, imaging such as X-rays or ultrasound is used to rule out fractures, inflammatory conditions, or other underlying issues. This comprehensive approach allows us to create a treatment plan tailored to your specific needs.
Bespoke Orthotics and Heel Pain Relief
For many patients, bespoke orthotics play a central role in treatment. Custom orthotics are designed specifically for your feet and your diagnosis. They provide precise arch support, improve foot alignment, and redistribute pressure away from painful areas.
Unlike over-the-counter insoles, bespoke orthotics are not generic. They are carefully crafted based on detailed measurements and assessments. When used correctly, they reduce strain on the plantar fascia, cushion the heel, and help prevent future episodes of pain.
Clinical evidence consistently shows high success rates for heel pain when custom orthotics are part of a comprehensive treatment plan.
Treatment Options for Heel Pain
Treatment depends entirely on the cause of your heel pain. For plantar fasciitis, treatment often includes bespoke orthotics, stretching programmes, footwear advice, and activity modification. In more persistent cases, shockwave therapy or corticosteroid injections may be recommended.
Heel pad syndrome requires cushioning and pressure redistribution, while Achilles-related pain focuses on controlled strengthening and load management. Stress fractures require rest and protected weight-bearing, whereas inflammatory conditions may need medical management alongside podiatric care.
Most patients experience significant improvement within weeks when treatment is properly matched to the diagnosis.
When to See a Podiatrist for Heel Pain
Heel pain should never be ignored. Early intervention leads to faster recovery and reduces the risk of long-term problems. If pain lasts longer than two weeks, worsens over time, keeps returning, or interferes with daily life, professional assessment is strongly advised.
Urgent care is needed if heel pain is accompanied by swelling, redness, numbness, night pain, fever, or difficulty bearing weight.
Take the First Step Towards Pain-Free Feet
Heel pain does not resolve on its own, and delaying treatment often leads to prolonged discomfort and limited treatment options. With expert diagnosis and evidence-based care, most heel pain can be successfully treated.
📞 Call Bucks Foot Clinic on 01494 434366 to book your comprehensive heel pain assessment today.
Our experienced podiatrists will identify the true cause of your pain and guide you toward lasting relief, helping you return to walking, exercising, and living comfortably again.
Life is too short to live with heel pain. Let Bucks Foot Clinic help you take the next step with confidence.
FAQ’s
Q: What causes heel pain?
A: Heel pain is usually caused by plantar fasciitis, tendon strain, inflammation, or stress on the foot.
Q: What is a heel spur?
A: A heel spur is a small bony growth on the heel that develops over time due to repeated stress.
Q: Do heel spurs always cause pain?
A: No. Many people have heel spurs without any pain.
Q: Why is heel pain worse in the morning?
A: The tissue under the foot tightens overnight, causing sharp pain with the first steps.
Q: Can heel pain go away on its own?
A: Mild cases may improve, but ongoing pain usually needs proper treatment.
Q: How is heel pain treated?
A: Treatment may include orthotics, stretching, footwear changes, shockwave therapy, or injections.
Q: When should I see a podiatrist?
A: If heel pain lasts more than a few weeks or affects daily activities.





Recent Comments