That persistent itch between your toes. The peeling, flaking skin. The burning sensation that just won’t go away. If you’re experiencing these symptoms, you’re likely dealing with athlete’s foot—one of the most common fungal infections affecting the feet, with up to 70% of the UK population experiencing it at some point in their lives.
Despite its name, athlete’s foot doesn’t only affect athletes. This contagious fungal infection can affect anyone, spreading easily in warm, moist environments and causing significant discomfort, embarrassment, and potential complications if left untreated. What begins as a minor irritation between the toes can progress to painful cracks, blisters, and even spread to your toenails, creating a much more challenging problem.
Understanding athlete’s foot its causes, effective treatments, and most importantly, why professional podiatric care often succeeds where home remedies fail is essential for achieving lasting relief and preventing recurrence.
If you’re struggling with persistent itching, burning, or peeling skin on your feet, don’t let this uncomfortable condition control your life. Contact Bucks Foot Clinic on 01494 434366 today for expert assessment and effective treatment. Our experienced podiatrists specialise in eliminating athlete’s foot and preventing its return.
What Is Athlete’s Foot?
Athlete’s foot, medically known as tinea pedis, is a fungal infection of the skin on the feet caused by dermatophyte fungi. These microscopic organisms thrive in warm, moist environments and feed on keratin—the protein found in skin, hair, and nails. The most common culprits are Trichophyton rubrum and Trichophyton mentagrophytes, the same fungi responsible for jock itch (tinea cruris) and fungal nail infections (onychomycosis).
The infection typically begins in the warm, damp spaces between the toes, particularly between the fourth and fifth toes, but can spread to other areas of the foot, including the soles, sides, and even the top of the foot. Without proper treatment, athlete’s foot can persist for months or even years, causing ongoing discomfort and serving as a source of infection that can spread to other body parts or other people.
Types of Athlete’s Foot
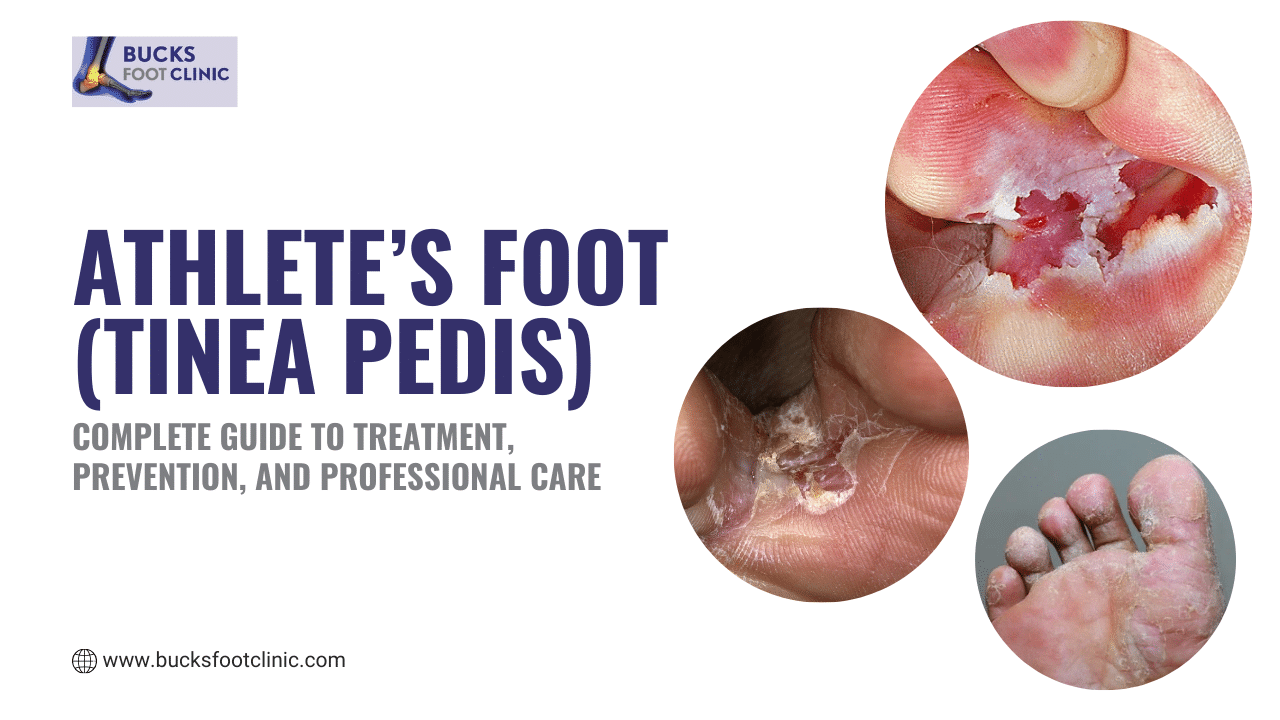
Athlete’s foot presents in several distinct forms, each with characteristic symptoms and challenges:
Interdigital (Toe Web) Athlete’s Foot is the most common type, accounting for approximately 75% of cases. This form affects the skin between the toes, particularly the fourth and fifth toes. The skin becomes macerated (white and soggy), itchy, and may develop painful cracks or fissures. The area often has a distinctive unpleasant odour. This type is most likely to develop secondary bacterial infections.
Moccasin-Type (Chronic Scaly) Athlete’s Foot affects the soles and sides of the feet in a “moccasin” distribution. This form causes dry, scaly skin that may appear silvery or white. The skin gradually thickens and may crack, particularly at the heels. Unlike other types, moccasin athlete’s foot is usually not itchy but can be uncomfortable. This is the most difficult type to treat and the most likely to spread to toenails.
Vesicular (Acute) Athlete’s Foot is the least common but most dramatic form. It causes sudden outbreaks of itchy, fluid-filled blisters (vesicles) on the soles, insteps, or between the toes. The blisters may be quite painful and can become infected if they rupture. This type often occurs in hot weather and may be triggered by occlusive footwear.
Ulcerative Athlete’s Foot is a severe, complicated form where bacterial infection occurs alongside the fungal infection. The skin between the toes breaks down, creating painful sores or ulcers. This type is more common in people with diabetes, compromised immune systems, or poor circulation.
Recognising the Symptoms
Athlete’s foot symptoms vary depending on the type but commonly include:
Itching and burning are usually the first symptoms noticed, particularly between the toes or on the soles. The itching can be intense and is often worse immediately after removing shoes and socks.
Redness and inflammation develop as the infection establishes, creating visibly irritated, inflamed skin in affected areas.
Scaling and peeling skin appears as the infection progresses, with dry, flaky skin that sheds continuously. The scales may be fine or coarse.
Cracking and fissures develop in the skin, particularly between toes or on heels. These painful cracks can bleed and create entry points for bacterial infections.
Maceration occurs when skin becomes waterlogged, appearing white, soggy, and wrinkled, particularly between toes.
Blisters may form in vesicular type, filled with clear fluid and often clustered together.
Thickening and discolouration of skin develops with chronic moccasin-type athlete’s foot.
Unpleasant odour often accompanies the infection, caused by both fungal activity and bacterial overgrowth.
Nail involvement may develop as the infection spreads from skin to toenails, causing thickening, discolouration, and crumbling.
What Causes Athlete’s Foot?
Understanding the causes and transmission of athlete’s foot is crucial for both treatment and prevention.
Primary Causes
Fungal organisms are ubiquitous in our environment. The dermatophyte fungi that cause athlete’s foot live on dead skin cells and thrive in warm, moist conditions. You can contract athlete’s foot from:
- Public swimming pools, showers, and changing rooms where infected skin cells contaminate floors
- Gym facilities and communal bathing areas
- Shared towels, bath mats, or footwear
- Hotel room floors and bathroom surfaces
- Spa and sauna facilities
- Contaminated nail salon equipment
- Direct contact with infected individuals
- Even your own home bathroom if someone in the household has the infection
Warm, moist environments create perfect conditions for fungal growth. The inside of shoes provides an ideal breeding ground—dark, warm, and often damp from perspiration.
Compromised skin barriers allow fungi to invade. Even microscopic breaks in the skin from friction, injury, or excessive moisture create entry points.
Risk Factors
Excessive foot sweating (hyperhidrosis) creates the moist environment fungi love. People whose feet sweat heavily are at significantly increased risk.
Occlusive footwear that doesn’t allow air circulation traps moisture against the skin. Wearing the same shoes daily without allowing drying time compounds the problem. Synthetic shoes and boots are particular culprits.
Wearing damp socks or shoes provides ideal fungal growing conditions. Walking in wet shoes or failing to change sweaty socks creates perfect environments for infection.
Walking barefoot in public areas exposes your feet directly to fungal organisms. Public showers, pool decks, and changing rooms are high-risk environments.
Sharing personal items including towels, socks, shoes, or nail clippers can transmit the infection between people.
Weakened immune system from medical conditions, medications, or stress reduces your body’s ability to fight off fungal infections.
Diabetes increases susceptibility through multiple mechanisms: reduced circulation, nerve damage affecting sensation, impaired immune response, and often dry, cracked skin that allows entry.
Age plays a role, with athlete’s foot more common in adults than children. However, it can affect any age group.
Gender influences risk slightly, with males more commonly affected than females, possibly due to footwear choices and activity patterns.
Previous fungal infections increase susceptibility. If you’ve had athlete’s foot before, you’re more likely to get it again.
Genetic predisposition exists for some individuals who appear more susceptible to dermatophyte infections.
Warm climates see higher infection rates due to increased foot sweating and more time in occlusive footwear.
Certain occupations carry higher risk, particularly those requiring:
- Prolonged wearing of heavy or rubber boots (construction workers, military personnel)
- Working in wet conditions (lifeguards, professional swimmers)
- Extended periods in athletic footwear (athletes, fitness instructors)
- Standing all day in enclosed shoes (healthcare workers, retail staff)
How to Prevent Athlete’s Foot: Your Essential Prevention Guide
Prevention is far easier than treatment, especially given athlete’s foot’s tendency to recur. These evidence-based strategies significantly reduce your risk:
Prevention Strategy #1: Keep Feet Clean and Dry
- Wash feet daily with soap and water, paying particular attention to spaces between toes
- Dry feet thoroughly after washing, especially between toes—this is crucial
- Consider using a hairdryer on cool setting to ensure complete drying between toes
- Apply foot powder or antifungal powder to absorb excess moisture
- Don’t go to bed with damp feet
Prevention Strategy #2: Choose and Manage Footwear Properly
- Wear shoes made from breathable materials like leather, canvas, or mesh
- Avoid synthetic materials that don’t allow air circulation
- Rotate shoes daily—never wear the same shoes two days consecutively
- Allow shoes at least 24 hours to dry completely between wearings
- Remove shoes whenever possible to allow feet to air
- Use shoe trees or stuff shoes with newspaper to absorb moisture and maintain shape
- Replace shoes that have become excessively worn or persistently smelly
- Consider open-toed shoes or sandals when appropriate
- Avoid tight shoes that compress toes together
Prevention Strategy #3: Select Appropriate Socks
- Choose moisture-wicking synthetic socks or wool rather than cotton
- Cotton absorbs moisture but holds it against skin—exactly what you don’t want
- Change socks at least daily, more frequently if feet sweat heavily or become damp
- Change socks immediately after exercise
- Consider antifungal socks if you’re prone to athlete’s foot
- Ensure socks fit properly without excessive bunching between toes
- Wash socks in hot water (60°C minimum) to kill fungal spores
Prevention Strategy #4: Protect Feet in Public Areas
- Always wear flip-flops, shower shoes, or water shoes in:
- Public showers and changing rooms
- Swimming pool areas and pool decks
- Gym facilities and fitness centre showers
- Hotel bathrooms
- Spa, sauna, and steam room facilities
- Communal bathing areas
- Never walk barefoot in these high-risk environments
- Wear water shoes even in the shower stalls
- Bring your own towel and avoid sharing
Prevention Strategy #5: Practice Good Hygiene
- Never share towels, socks, shoes, or nail implements
- Wash bath mats frequently in hot water
- Disinfect shower floors regularly, especially if someone in the household has athlete’s foot
- Use separate towels for feet if you’re prone to infection
- Keep toenails trimmed short and clean
- Remove dead skin regularly but gently—excessive removal can create entry points
Prevention Strategy #6: Manage Foot Sweating
- Use antiperspirant on feet if you sweat heavily—yes, this works!
- Apply antiperspirant to soles and between toes before bed
- Consider prescription-strength antiperspirants if over-the-counter products are insufficient
- Use absorbent foot powder during the day
- Explore medical treatments for hyperhidrosis if sweating is severe
Prevention Strategy #7: Avoid Prolonged Damp Conditions
- Change out of wet shoes and socks immediately
- Dry feet and change socks if they become damp during the day
- Remove shoes and socks as soon as possible after exercise
- Don’t wear the same exercise shoes multiple days running
- Use moisture-absorbing insoles in athletic shoes
Prevention Strategy #8: Strengthen Your Immune System
- Maintain good overall health through balanced diet and regular exercise
- Manage chronic conditions like diabetes carefully
- Get adequate sleep—immune function suffers with poor sleep
- Manage stress levels
- Avoid smoking, which impairs circulation and immune function
Prevention Strategy #9: Treat Any Infection Promptly and Completely
- Address athlete’s foot at the first sign
- Complete the full course of treatment even after symptoms resolve
- Continue treatment for 1-2 weeks beyond symptom resolution to prevent recurrence
- Treat all affected areas, not just the most symptomatic spots
Prevention Strategy #10: Be Cautious with Nail Salons and Spas
- Choose establishments with visible sterilisation procedures
- Watch for proper cleaning of foot baths between clients
- Consider declining foot razors or callus removal tools that can create entry points
- Bring your own implements if possible
Prevention Strategy #11: Manage Risk Factors
- Control blood sugar if diabetic
- Address circulatory problems with medical care
- Treat any skin conditions that affect feet
- Maintain healthy foot skin—not too dry (cracks allow entry) but not too moist
Prevention Strategy #12: Use Preventive Antifungal Products
- Apply antifungal powder to feet and in shoes if you’re high-risk
- Use antifungal spray in shoes regularly
- Consider preventive antifungal cream once weekly if you’ve had recurrent infections
- Treat shoes with antifungal spray or UV sanitisers
Want personalised advice on preventing athlete’s foot based on your specific lifestyle and risk factors? Call Bucks Foot Clinic on 01494 434366 to schedule a foot health consultation. We’ll assess your individual risks and create a tailored prevention strategy.
Home Remedies for Athlete’s Foot: Understanding Their Limitations
Many people attempt to treat athlete’s foot at home, and some remedies may provide temporary relief. However, it’s crucial to understand their limitations and why they often fail or provide only partial success.
Over-the-Counter Antifungal Creams
What they are: Products containing clotrimazole, miconazole, terbinafine, or tolnaftate available without prescription.
Reality and limitations: These are actually reasonably effective for mild, early-stage athlete’s foot if used properly. However:
- Most people don’t use them long enough—treatment must continue for 2-4 weeks beyond symptom resolution
- Application must be thorough, covering all affected areas and surrounding skin
- They work best for interdigital athlete’s foot, less well for moccasin type
- Success rates vary widely (40-70%) depending on compliance and infection severity
- Reinfection is common if environmental factors aren’t addressed
- They won’t work if there’s also a bacterial infection
- Many people stop too soon when symptoms improve, leading to recurrence
- They cannot treat fungal nail infections that may be seeding ongoing foot infection
Tea Tree Oil
What it claims: Natural antifungal properties can cure athlete’s foot.
Reality and limitations: Tea tree oil does have antifungal properties, but evidence is limited. A few small studies show some benefit, but it’s not as effective as standard antifungals. It must be used at high concentrations (25-50%), which can cause skin irritation. It takes longer to work than conventional treatments. It may help mild cases but is insufficient for established infections. Can cause allergic reactions in some people. The smell is distinctive and not everyone finds it pleasant.
Vinegar Soaks
What it claims: The acidic environment created by vinegar kills fungi.
Reality and limitations: Whilst vinegar creates an inhospitable environment for some organisms, dermatophytes can survive acidic conditions. There’s very limited scientific evidence supporting vinegar for athlete’s foot. It might provide temporary relief from itching but rarely cures the infection. Prolonged soaks can dry and damage skin, potentially worsening the condition. Any benefit is likely from the cleaning and drying effect rather than antifungal action. It’s inconvenient—requiring 15-30 minute soaks daily.
Baking Soda
What it claims: Neutralises foot odour and has antifungal properties.
Reality and limitations: Baking soda is good at neutralising odour but has minimal antifungal activity. It may help keep feet dry by absorbing moisture but doesn’t cure the infection. It can cause skin irritation with excessive use. There’s no credible evidence it’s effective against dermatophyte fungi. At best, it’s an adjunct to reduce symptoms, not a cure.
Garlic
What it claims: Natural antifungal compounds in garlic cure athlete’s foot.
Reality and limitations: Whilst garlic has some antifungal properties in laboratory settings, applying it to skin is problematic. Raw garlic is highly irritating and can cause chemical burns. The compounds that might have antifungal effects can damage skin before killing fungi. There’s no good clinical evidence supporting this treatment. The smell is socially unacceptable. Risk of harm outweighs any potential benefit.
Hydrogen Peroxide
What it claims: Kills fungi through oxidative action.
Reality and limitations: Hydrogen peroxide has some antimicrobial activity but limited antifungal effect against dermatophytes. It can irritate and dry skin with repeated use. It may help prevent secondary bacterial infection but doesn’t effectively treat the fungal infection. Not recommended by podiatrists as a primary treatment.
Saltwater Soaks
What they claim: Salt draws out moisture and kills fungi.
Reality and limitations: Salt soaks may temporarily reduce moisture and provide symptomatic relief but don’t cure athlete’s foot. They can help clean the area and reduce odour. Some people find them soothing. However, they don’t have significant antifungal activity. Excessive use can dry skin excessively, leading to cracking. They’re time-consuming and inconvenient.
Keeping Feet Dry
What it does: Removes the moist environment fungi need.
Reality and limitations: This is actually crucial and works well as a preventive measure and treatment adjunct. However, keeping feet dry alone rarely cures established athlete’s foot. The fungi are already present and embedded in the skin. Drying helps prevent worsening and spread but doesn’t eliminate existing infection. It’s essential but insufficient as a sole treatment.
The Fundamental Problem with Relying Solely on Home Remedies
Here’s the critical issue: mild athlete’s foot caught very early might respond to OTC antifungals, but most people don’t seek any treatment until the infection is well-established. By that point:
- The fungus has penetrated deeper into skin layers
- Multiple areas may be affected
- Fungal nail infection may have developed, creating a reservoir for reinfection
- Secondary bacterial infection may be present
- Skin damage (cracks, fissures) has occurred
- The infection has had time to spread in the environment (shoes, floors, towels)
Home treatment often fails because:
- Treatment is started too late
- Application is incomplete or inconsistent
- Treatment duration is too short
- Environmental decontamination is neglected
- Fungal nail reservoirs aren’t addressed
- Underlying risk factors aren’t managed
- Reinfection occurs from contaminated footwear or environment
- Diagnosis is wrong—it’s not actually athlete’s foot
Why a Podiatrist Is Better Than Home Remedies
Professional podiatric care offers comprehensive assessment, accurate diagnosis, and access to treatments and expertise that home remedies cannot match. Here’s why seeing a podiatrist at Bucks Foot Clinic is essential for persistent or recurrent athlete’s foot:
Accurate Diagnosis
Not all itchy, scaly, or peeling foot skin is athlete’s foot. Conditions that can mimic athlete’s foot include:
- Contact dermatitis from shoes, socks, or foot products
- Eczema or atopic dermatitis
- Psoriasis of the feet
- Dyshidrotic eczema (pompholyx)
- Bacterial infections (sometimes coexisting with fungal infection)
- Erythrasma (bacterial infection)
- Juvenile plantar dermatosis
- Allergic reactions
Treating the wrong condition wastes time and money whilst the real problem persists or worsens. At Bucks Foot Clinic, we can:
- Perform thorough clinical examination
- Assess skin appearance, distribution, and characteristics
- Take skin scrapings for laboratory analysis when diagnosis is uncertain
- Identify whether fungal, bacterial, or both types of infection are present
- Recognise differential diagnoses
- Provide definitive diagnosis through testing
This diagnostic accuracy is impossible with self-treatment.
Access to Prescription-Strength Medications
Podiatrists can prescribe medications unavailable over the counter that are more effective for moderate to severe athlete’s foot:
Prescription-Strength Topical Antifungals:
- Econazole 1% cream
- Ketoconazole 2% cream
- Terbinafine 1% cream (available OTC but prescription-strength formulations exist)
- Ciclopirox cream
- Naftifine cream
These prescription products often contain higher concentrations or different formulations that penetrate better and work more effectively.
Topical Corticosteroids: For severely inflamed athlete’s foot, we may prescribe combination products containing both antifungal and anti-inflammatory corticosteroids to:
- Reduce inflammation and itching quickly
- Improve patient comfort during antifungal treatment
- Reduce the inflammatory component that can impair healing
These must be used carefully and for limited duration under professional supervision.
Oral Antifungal Medications: For severe, widespread, or resistant athlete’s foot, oral antifungals may be necessary:
- Terbinafine tablets: Highly effective for dermatophyte infections, typically 2-4 week course
- Itraconazole capsules: Alternative for resistant cases
- Fluconazole: Sometimes used for yeast infections
Oral medications work systemically, treating infection from inside the body. They’re particularly important when:
- Fungal nail infection is present (common with chronic athlete’s foot)
- Moccasin-type athlete’s foot hasn’t responded to topical treatment
- Infection is widespread or severe
- Multiple sites are affected
- Patient has recurrent infections despite proper topical treatment
Podiatrists assess your suitability for oral medications, monitor for side effects, and ensure safe, effective treatment.
Antibiotics for Secondary Bacterial Infection: Ulcerative athlete’s foot or severely cracked skin often develops bacterial infection. We can prescribe appropriate antibiotics to treat concurrent bacterial infection whilst managing the underlying fungal problem.
Professional Skin Care and Debridement
At Bucks Foot Clinic, we provide professional skin care that enhances treatment:
- Removal of dead, infected skin that harbours fungi
- Treatment of hyperkeratosis (thickened skin) in moccasin-type athlete’s foot
- Safe management of blisters in vesicular type
- Professional drying and cleaning of affected areas
- Application of prescription treatments in the correct manner
This professional care accelerates healing and improves treatment penetration.
Treatment of Fungal Nail Infections
One of the most common reasons athlete’s foot keeps returning is undiagnosed or untreated fungal nail infection. The infected nails serve as a reservoir, continuously re-seeding skin infection even after successful topical treatment.
At Bucks Foot Clinic, we:
- Examine all toenails carefully for signs of infection
- Diagnose fungal nail infections early
- Treat nail and skin infections simultaneously
- Prevent the cycle of reinfection from nails to skin
- Provide comprehensive care addressing all fungal problems
This integrated approach dramatically improves success rates and reduces recurrence—something impossible with self-treatment focused only on skin symptoms.
Identification and Management of Risk Factors
Professional assessment identifies why you developed athlete’s foot and why it keeps recurring:
Biomechanical factors:
- Foot structure causing excessive sweating in certain areas
- Toe crowding or overlap creating persistently moist pockets
- Gait abnormalities affecting pressure and friction
Footwear problems:
- Inappropriate shoe choices for foot type or activity
- Poor shoe fit creating friction or moisture retention
- Inadequate shoe rotation allowing persistent dampness
Systemic factors:
- Undiagnosed diabetes or prediabetes
- Circulatory problems requiring medical attention
- Immune system issues
- Hyperhidrosis needing specific treatment
Lifestyle factors:
- Occupation or activities creating high-risk exposure
- Environmental factors in home or work
- Personal hygiene practices needing modification
We provide tailored advice addressing your specific risk factors, dramatically reducing recurrence risk.
Comprehensive Decontamination Protocols
Successful treatment requires eliminating fungi from your environment, not just your feet. We provide detailed guidance on:
Footwear management:
- Which shoes need replacing vs decontaminating
- Effective shoe treatment methods (sprays, UV sanitisers)
- Shoe rotation schedules
- Choosing appropriate footwear for foot type and activities
Home environment:
- Proper bathroom disinfection
- Laundry protocols for socks and towels
- Treating carpets and floors if necessary
- Family education to prevent spread
Personal items:
- Nail clipper sterilisation
- Bath mat management
- Towel hygiene
This comprehensive approach addresses all sources of reinfection.
Treatment Plans for Recurrent Athlete’s Foot
If you’ve had athlete’s foot multiple times, simple OTC treatment clearly isn’t working. We develop comprehensive management plans including:
- Investigation and treatment of underlying predisposing factors
- Prophylactic antifungal strategies
- Environmental control measures
- Regular monitoring and maintenance care
- Long-term prevention protocols
Struggling with persistent or recurrent athlete’s foot that won’t respond to over-the-counter treatments? Stop the cycle of recurrence. Call Bucks Foot Clinic on 01494 434366 today for comprehensive assessment and effective treatment. We’ll identify why it keeps coming back and create a plan to eliminate it for good.
How to Fix Athlete’s Foot: Comprehensive Treatment Options
Effective athlete’s foot treatment requires the right diagnosis, appropriate medications, adequate duration, and addressing all contributing factors. Here’s what professional treatment at Bucks Foot Clinic involves:
Step 1: Accurate Diagnosis and Assessment
Treatment begins with accurate diagnosis through:
- Clinical examination of all affected areas
- Assessment of infection type and severity
- Checking for concurrent nail infections
- Laboratory testing if diagnosis is uncertain or treatment has failed
- Evaluation of risk factors and predisposing conditions
- Assessment of footwear and lifestyle factors
Step 2: Treatment Selection Based on Infection Type and Severity
For Mild Interdigital Athlete’s Foot
Topical Antifungal Treatment:
- Prescription-strength or quality OTC antifungal cream
- Apply twice daily to affected areas and surrounding skin
- Treatment duration: Minimum 2-4 weeks, continuing 1-2 weeks beyond symptom resolution
- Common choices: Terbinafine 1% cream, clotrimazole 1% cream, miconazole 2% cream
Adjunct Measures:
- Keep affected areas clean and dry
- Use absorbent powder between toes
- Wear appropriate footwear and socks
- Change socks 1-2 times daily
Expected Timeline:
- Symptom improvement within 3-7 days
- Significant improvement by 2 weeks
- Complete resolution by 3-4 weeks
For Moderate to Severe Interdigital Athlete’s Foot
Enhanced Topical Treatment:
- Prescription-strength antifungal (econazole, ketoconazole, or terbinafine)
- Possible short-term combination with mild corticosteroid for inflammation
- More frequent application (2-3 times daily initially)
- Extended treatment duration (4-6 weeks)
If Secondary Bacterial Infection Present:
- Oral antibiotics (flucloxacillin, erythromycin, or amoxicillin)
- Treatment typically 7-14 days
- Continue antifungal treatment throughout
Additional Professional Care:
- Debridement of macerated skin
- Professional drying and cleaning
- Guidance on managing severely affected areas
For Moccasin-Type (Chronic) Athlete’s Foot
This type is the most challenging to treat and often requires:
Oral Antifungal Medications:
- Terbinafine 250mg daily for 2-4 weeks (sometimes longer)
- Most effective for dermatophyte infections
- Requires liver function monitoring
- Success rates: 70-80% when combined with other measures
OR
- Itraconazole 200mg twice daily for 1 week (pulse therapy)
- Alternative for resistant cases
- Also requires monitoring
Combined with Topical Treatment:
- Prescription-strength topical antifungal cream
- Applied daily throughout oral treatment and beyond
- Helps prevent recurrence
Professional Debridement:
- Removal of thick, scaly skin
- Allows better medication penetration
- Performed every 4-6 weeks during treatment
- Significantly enhances treatment effectiveness
Keratolytic Agents:
- Urea cream (10-40%) to soften thick skin
- Salicylic acid preparations when appropriate
- Facilitates penetration of antifungals
Concurrent Nail Treatment:
- Moccasin-type athlete’s foot commonly spreads to nails
- Nail infection must be treated simultaneously
- Oral antifungals treat both nail and skin
- Prevents continuous reinfection from nails
Treatment Duration:
- Often requires 6-12 weeks of treatment
- May need extended or intermittent therapy
- Recurrence is common without proper maintenance
For Vesicular (Acute) Athlete’s Foot
Initial Management:
- Drying agents to reduce blistering (Burow’s solution compresses)
- Short-term corticosteroids to reduce severe inflammation and itching
- Antifungal treatment begins after acute phase settles
Antifungal Treatment:
- Topical antifungals once acute inflammation controlled
- Duration: 4-6 weeks minimum
- Continue beyond symptom resolution
Prevent Secondary Infection:
- Keep blisters intact when possible
- Sterile drainage if necessary
- Monitor for signs of bacterial infection
- Antibiotics if infection develops
For Ulcerative Athlete’s Foot
This severe form requires aggressive treatment:
Oral Antibiotics:
- First-line treatment for bacterial infection
- 10-14 day course typically
- Commonly flucloxacillin or co-amoxiclav
Oral Antifungal Medications:
- Started after bacterial infection controlled
- Terbinafine or itraconazole
- Full treatment course essential
Wound Care:
- Professional cleaning and debridement
- Appropriate dressings
- Regular monitoring
- Education on proper foot care
Management of Underlying Conditions:
- Diabetes optimization
- Circulatory assessment
- Immune system evaluation
Step 3: Comprehensive Adjunct Measures
Alongside primary medical treatment, successful management requires:
Footwear Management:
- Treat or replace all regularly worn shoes
- Use antifungal sprays in shoes daily during treatment
- Consider UV shoe sanitisers
- Rotate shoes with minimum 24-hour drying time
- Choose breathable footwear
Sock Protocol:
- Change socks 1-2 times daily during active infection
- Wash in hot water (60°C minimum)
- Use moisture-wicking synthetic or wool socks
- Consider antifungal socks
Hygiene Measures:
- Wash feet twice daily with antifungal or antibacterial soap
- Dry thoroughly, especially between toes
- Use separate towel for feet
- Disinfect bathroom regularly
Environmental Decontamination:
- Disinfect shower/bath with bleach solution weekly
- Wash bath mats in hot water frequently
- Vacuum and clean floors regularly
- Address any damp problems in home
Moisture Control:
- Apply antifungal powder to feet and in shoes
- Use antiperspirant on feet if sweating is problematic
- Remove shoes whenever possible to air feet
- Consider moisture-absorbing insoles
Step 4: Monitoring and Follow-Up
Professional treatment includes regular monitoring:
Week 1-2:
- Assess treatment response
- Evaluate for side effects or allergic reactions
- Reinforce compliance and proper application technique
- Adjust treatment if inadequate response
Week 3-4:
- Should see significant improvement
- Continue treatment even after symptoms resolve
- Plan for extended treatment if needed
- Begin discussing maintenance strategies
Week 4-8:
- Complete treatment course
- Assess for complete resolution
- Screen for nail involvement
- Implement prevention protocols
Long-term:
- Periodic monitoring if recurrence risk is high
- Maintenance strategies as needed
- Address any new occurrences promptly
Step 5: Managing Expectations
Realistic Timelines:
- Symptom improvement: Usually within 3-7 days
- Significant improvement: 1-2 weeks
- Complete resolution: 2-6 weeks depending on type and severity
- Moccasin type: Often requires 6-12 weeks
Success Rates with Proper Treatment:
- Mild interdigital athlete’s foot: 80-90% cure with topical treatment
- Moderate athlete’s foot: 70-85% cure with enhanced treatment
- Moccasin-type: 70-80% cure with oral antifungals plus topical therapy
- Vesicular type: 75-85% cure with appropriate management
Factors Affecting Outcomes:
- Compliance with treatment regimen
- Concurrent nail infection treatment
- Environmental decontamination
- Management of risk factors
- Proper footwear and hygiene
- Underlying health conditions
Preventing Recurrence: Long-Term Strategies
After successful treatment, preventing recurrence is essential:
Maintenance Antifungal Treatment:
- Weekly application of antifungal cream
- Antifungal powder in shoes regularly
- Consider prophylactic treatment during high-risk periods
Ongoing Hygiene:
- Continue excellent foot hygiene practices
- Maintain proper footwear rotation and care
- Use preventive measures in high-risk environments
- Regular nail care and monitoring
Risk Factor Management:
- Control foot sweating
- Choose appropriate footwear
- Manage underlying health conditions
- Maintain good overall health
Early Intervention:
- Treat any recurrence immediately
- Don’t wait for symptoms to worsen
- Keep antifungal cream on hand
- Contact podiatrist if home treatment doesn’t resolve quickly
Regular Podiatric Care:
- Annual foot health checks
- Periodic monitoring if high-risk
- Professional advice on prevention
- Early detection of problems
Ready to eliminate athlete’s foot once and for all? Call Bucks Foot Clinic on 01494 434366 to schedule your comprehensive assessment. Our podiatrists will diagnose your specific type of athlete’s foot, create an effective treatment plan, and help you prevent recurrence with evidence-based strategies.
When to See a Podiatrist for Athlete’s Foot
Many people wonder when home treatment is appropriate versus when professional care is necessary. Here’s guidance:
See a Podiatrist When:
Your first episode of athlete’s foot – Professional diagnosis ensures you’re treating the right condition and establishes proper treatment from the start.
Symptoms haven’t improved within 2 weeks of OTC treatment – If proper home treatment with quality antifungal cream hasn’t produced noticeable improvement, professional assessment is needed.
The infection keeps coming back – Recurrent athlete’s foot indicates underlying problems that need professional identification and management.
The infection is spreading – If athlete’s foot is spreading to other areas of your feet, other people, or other body parts, professional treatment is essential.
You have thick, scaly soles – Moccasin-type athlete’s foot rarely responds to OTC treatment alone and typically requires oral antifungals.
You have blisters or severe inflammation – Vesicular athlete’s foot needs professional management to prevent complications and speed resolution.
There are cracks, sores, or raw areas – Broken skin can lead to bacterial infection and requires professional care.
You notice signs of infection – Increased pain, redness, swelling, pus, red streaks, or fever indicate possible bacterial infection requiring urgent treatment.
You have diabetes – Any foot problem in diabetic patients requires professional podiatric care to prevent serious complications.
You have circulatory problems – Poor circulation increases infection risk and impairs healing, necessitating professional management.
You have a weakened immune system – From any cause, immunosuppression makes fungal infections more serious and harder to treat.
Your toenails are thick, discoloured, or crumbling – This suggests fungal nail infection that won’t respond to treatment for athlete’s foot skin infection alone.
You want to prevent recurrence – Professional assessment identifies your specific risk factors and creates personalised prevention strategies.
You’re unsure if it’s athlete’s foot – If symptoms are atypical or diagnosis is uncertain, professional evaluation is essential.
Don’t Wait If You Experience:
Severe pain – Significant pain suggests possible bacterial infection or complications requiring urgent care.
Rapidly worsening symptoms – Fast progression indicates aggressive infection or incorrect diagnosis needing immediate assessment.
Fever or feeling unwell – Systemic symptoms suggest serious infection requiring prompt medical attention.
Red streaks – Red lines extending from the affected area indicate spreading infection (lymphangitis) requiring urgent antibiotic treatment.
Extensive swelling – Significant swelling beyond the immediate area of athlete’s foot suggests cellulitis requiring urgent treatment.
Black or dead-appearing tissue – Any tissue that appears black, grey, or dead requires emergency medical attention, particularly for diabetics.
The Bucks Foot Clinic Approach to Athlete’s Foot
At Bucks Foot Clinic, we understand that athlete’s foot is more than just an annoying itch—it can significantly impact your comfort, confidence, and quality of life. Our comprehensive approach to athlete’s foot treatment includes:
Thorough Diagnostic Assessment
We don’t assume every itchy foot is athlete’s foot. Our comprehensive examination:
- Carefully evaluates all affected areas
- Assesses infection type and severity
- Examines all toenails for concurrent infection
- Considers differential diagnoses
- Performs laboratory testing when needed
- Identifies underlying risk factors
Evidence-Based Treatment Selection
We focus exclusively on treatments with robust scientific evidence:
- Proven antifungal medications
- Appropriate treatment duration based on infection type
- Combination therapy when beneficial
- Avoiding trendy but unproven remedies
Personalised Treatment Plans
We recognise every patient is unique:
- Treatment matched to your specific infection type
- Consideration of your medical history and medications
- Respect for your preferences and lifestyle
- Addressing your individual risk factors
- Realistic goal-setting based on your situation
Comprehensive Care Beyond Medication
Successful treatment requires more than just prescribing cream:
- Professional skin care and debridement when needed
- Detailed footwear and hygiene guidance
- Environmental decontamination protocols
- Treatment of concurrent nail infections
- Management of hyperhidrosis if present
- Addressing biomechanical factors when relevant
Honest Communication
We provide realistic expectations:
- Accurate information about treatment duration
- Honest discussion of success rates
- Clear explanation of recurrence risks
- Transparency about costs
- Straightforward advice on what works and what doesn’t
Ongoing Support
Athlete’s foot management extends beyond initial treatment:
- Regular monitoring during treatment
- Adjustments to protocols based on response
- Long-term prevention strategies
- Availability for recurrence concerns
- Partnership in maintaining foot health
Patient Education
We believe informed patients achieve better outcomes:
- Clear explanation of why you developed athlete’s foot
- Teaching proper treatment application techniques
- Education on prevention strategies
- Empowerment to recognize and address problems early
- Resources for maintaining foot health
Don’t let athlete’s foot control your life. Take the first step towards healthy, comfortable feet today. Call Bucks Foot Clinic on 01494 434366 to schedule your comprehensive athlete’s foot assessment. Our experienced podiatrists will accurately diagnose your condition, create an effective treatment plan, and help you maintain healthy feet for the long term.
Living Well with Healthy Feet
Athlete’s foot is one of the most common foot problems, but it doesn’t have to be a recurring nightmare. With accurate diagnosis, appropriate treatment, environmental management, and professional guidance, you can eliminate athlete’s foot and prevent its return.
The key is not accepting athlete’s foot as an inevitable inconvenience. It’s a treatable medical condition that responds well to proper professional care. Whether you’re dealing with your first episode or your tenth recurrence, professional podiatric care offers solutions that self-treatment often cannot.
Don’t let embarrassment, inconvenience, or hoping it will resolve on its own delay effective treatment. The longer athlete’s foot persists, the more difficult it becomes to treat, the more likely it spreads to nails, and the greater the risk of complications.
Bucks Foot Clinic: Expert diagnosis, effective treatment, and personalised prevention strategies for athlete’s foot. Call 01494 434366 today.
Bucks Foot Clinic: Where evidence-based care meets compassionate service. Your foot health is our priority.
FAQ’s
Q: What is athlete’s foot?
A: Athlete’s foot is a fungal infection that affects the skin of the feet, often between the toes.
Q: What causes athlete’s foot?
A: It is caused by fungi that grow in warm, moist places like sweaty shoes and communal showers.
Q: What are the common symptoms?
A: Itching, burning, peeling or flaky skin, cracks, and sometimes blisters.
Q: Is athlete’s foot contagious?
A: Yes, it can spread through direct contact or shared surfaces.
Q: How can athlete’s foot be prevented?
A: Keep feet clean and dry, change socks daily, wear breathable shoes, and avoid walking barefoot in public areas.
Q: How is athlete’s foot treated?
A: Treatment usually includes antifungal creams, sprays, or powders.
Q: When should I see a podiatrist?
A: If symptoms don’t improve, keep coming back, or if you have diabetes.



